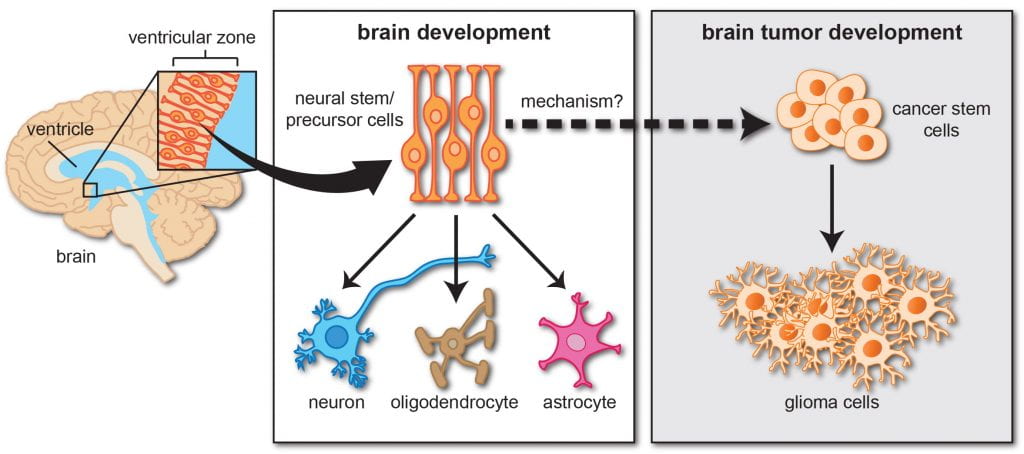
Over the past several years, there has been a growing appreciation for the role of neurons in brain tumor initiation and growth (“cancer neuroscience”). Using genetically engineered mouse models of neurofibromatosis type 1 (NF1) optic glioma, we demonstrated that NF1 mutation increases the excitability of neurons that course through the optic nerve (retinal ganglion cells). This neuronal hyperexcitability directs both tumor initiation and progression through at least three independent mechanisms.
First, in collaboration with Dr. Michelle Monje (link to her website), we showed that light (visual experience) controls tumor initiation by regulating Adam10-mediated cleavage of neuroligin-3 (Nlgn3) on oligodendroglial cells. In this manner, dark rearing optic glioma mice reduced soluble Nlgn3 protein levels and abrogated tumor formation.
Second, Dr. Corina Anastasaki found that NF1 mutation additionally increases baseline retinal ganglion cell excitability. This mechanism involves a specific ion (HCN) channel, which can be reversed by drugs like lamotrigine, a drug commonly used to treat children with epilepsy. HCN-mediated neuronal hyperexcitability in brain neurons leads to increased midkine production, which controls T cell-mediated immune support of optic glioma growth – one of the first demonstrations that neurons can control immune cell function in the brain. Leveraging these findings, Dr. Jit Chatterjee found that midkine is essential for Nf1 optic glioma growth. Importantly, lamotrigine blocks tumor growth at doses lower than used for children with epilepsy and is effective at inhibiting tumor progression, setting the stage for future clinical trials.
Similar to its effects in brain neurons, NF1 mutation also induces hyperexcitability in peripheral sensory neurons (dorsal root ganglion cells). Instead of controlling T cell function, these hyperactive neurons produce collagen to directly increase peripheral nerve tumor (plexiform neurofibroma) growth.
In addition, the effect of NF1 mutation on neuronal hyperexcitability and midkine production is mutation-specific, raising the intriguing possibility that neuronal excitability and serum midkine levels might be useful biomarkers for tumor predisposition in these at-risk children.
Third, emerging work by Dr. Anastasaki has shown differential effects of neurotransmitters and neurotransmitter receptor inhibitors on tumor growth, expanding the underlying mechanisms by which nerves control tumor formation and progression.
Current projects in the Gutmann laboratory are focused on determining (1) how neurons control brain and nerve tumor initiation and growth, (2) how neuronal hyperexcitability is dictated by cancer causing genetic mutations, and (3) the role of neurotransmitters in selectively regulating pediatric glioma growth.